COVID-19 and atrial fibrillation
How does coronavirus affect people with atrial fibrillation?
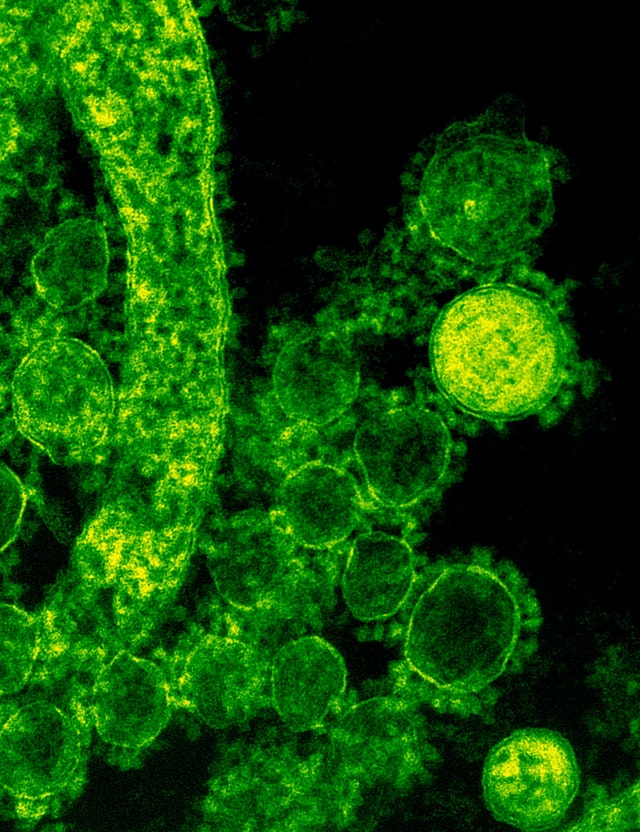
Since February 2020, coronavirus has affected everyone’s lives. In the meantime, most people got infected by the SARS-CoV-2 virus and built immunity against the pathogen resulting in less severe illness. However, much remains uncertain about the virus. Nevertheless, there is still notably uncertainty surrounding the virus. For example, what risks are there for people with atrial fibrillation?
What is known so far about COVID-19 and atrial fibrillation:
- People with risk factors for atrial fibrillation are left quite vulnerable after being infected with the coronavirus
- High blood pressure, diabetes, obesity, and narrowed coronary arteries are all risk factors often associated with severe COVID-19 symptoms
- There is a possible link between COVID-19 and drugs for hypertension and high blood pressure
- Researchers across Europe collaborate on heart disease and COVID-19
COVID-19 vulnerability to certain risk factors
People with underlying conditions have a greater chance of serious corona symptoms when infected with the virus. This may happen even if they are fully vaccinated. High blood pressure, diabetes, and narrowing of the coronary arteries are risk factors for people with atrial fibrillation. People with these risk factors are also more likely to have suffer severely of COVID-19.
A recent study from Israel shows that 152 vaccinated (older) people who were hospitalized had the following underlying conditions:
- High blood pressure (71%)
- Diabetes (48%)
- Heart failure (27%)
- Kidney and lung disorders (24%)
- Dementia (19%)
- Cancer (24%)
- Failing immune system (40%)
Here too, a healthy lifestyle can make the difference.
The impact of COVID-19 on the heart
Coronavirus enters your body by binding itself to the ACE2 protein. This protein can be found mainly in the cell membrane of your lungs, heart, kidneys, blood vessels, and gut. Therefore, these organs are overly vulnerable when you have had corona. They can even suffer actual damage.
High blood pressure medications are not a risk
As mentioned above, coronavirus enters the body by binding to the ACE2 protein. High blood pressure drugs such as ACE inhibitors and angiotensin receptor inhibitors (ARB) may increase ACE2. But, does this also mean that COVID-19 can damage more cells? Study results now show that the use of high blood pressure drugs has no influence on the disease process of the coronavirus.
The aftermath of coronavirus on the heart
People may still experience symptoms months after being infected with coronavirus. Additionally, heart problems may also occur. These are mainly caused by blood vessels closing due to blood clotting. There is no blood rich in oxygen directed towards the heart cells, and as a result, the heart functions less optimally.
Moreover, the body also has an excessive immune response to infected cells. This is called a cytokine storm. A cytokine storm then causes myocarditis. The latter consisting of a breakdown of heart cells and subsequent inflammatory reactions in the heart.
Atrial fibrillation after a corona vaccination
Some of our patient collaborators admitted to have had an atrial fibrillation attack after their corona vaccination. There has been virtually no report nor investigation made regarding this issue in medical literature. So far there has been only one case study regarding a combination of atrial fibrillation, anticoagulation and bleeding under the skin after vaccination with Oxford-AstraZeneca Covid-19 vaccine.
Share this article