Can Vitamin D Lower Your Risk of Atrial Fibrillation? Exploring the Link Between Heart Health and the Sunshine Vitamin
Researchers are increasingly highlighting the impact of vitamin D on cardiac health. Recent studies suggest that adequate vitamin D levels may lower the risk of atrial fibrillation (Afib) and that a deficiency could potentially be a risk factor. For individuals at risk for cardiovascular issues, including those with hypertension or a history of inflammation, maintaining adequate vitamin D levels could offer significant cardiovascular benefits.
Key points:
The main takeaways of this article are:
- Keeping vitamin D at healthy levels is linked to a lower risk of atrial fibrillation and may benefit heart health, especially for those with high blood pressure or inflammation.
- Vitamin D boosts calcium absorption and, combined with calcium supplements, can raise HDL (“good” cholesterol) and lower blood pressure, both linked to a reduced risk of Afib.
- Vitamin D helps regulate the renin-angiotensin-aldosterone system (RAAS), a key system for blood pressure control, potentially reducing the risk of Afib linked to high blood pressure.
The role of Vitamin D in the body
Vitamin D is an important nutrient that can be either ingested through foods rich in this vitamin such as fatty fish, milk, and mushrooms, or synthesized from the ultraviolet rays of the sun. Vitamin D has multiple roles in our bodies some of which include:
- maintaining bone health by aiding in calcium absorption
- ensuring normal muscle growth and development
- regulating blood pressure
- regulating vascular cell growth
- regulating inflammatory and fibrotic pathways
Additionally, a Vitamin D deficiency has been associated with arterial stiffening, left ventricular hypertrophy, vascular dysfunction, and hyperlipidemia. Thus this vitamin is very important when it comes to heart health.
Now let’s look at these mechanisms in more detail to understand the protective effects of vitamin D.
Vitamin D increases calcium absorption
Vitamin D promotes the intestinal absorption of calcium and they are often prescribed together to boost this effect. Though an increased serum calcium concentration has been seen to possibly increase the risk of cardiovascular disease, dietary supplementation has not been seen to have this negative effect. A randomized controlled trial found that calcium supplementation could have favorable effects on the fats circulating in our blood, in menopausal women. The amount of “good cholesterol” (HDL) increased by 7%. A systematic review that investigated 42 trials with calcium supplementation found that systolic blood pressure decreased by 1.44 mm Hg and diastolic blood pressure dropped by 0.84 mm Hg. Vitamin D could further promote these positive effects but further research is needed in this particular field.
Low HDL cholesterol has been associated with an increased risk of Afib and thus the positive effects of calcium supplementation on and vitamin D are of great interest.
How vitamin D influences blood pressure
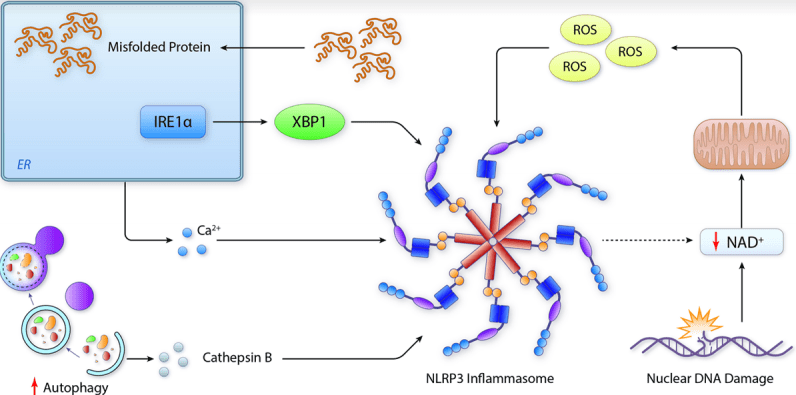
The most pivotal role of vitamin D for cardiovascular health is in the regulation of the renin-angiotensin-aldosterone system (RAAS). As seen from the image, this system is involved with regulating blood pressure. Renin from the kidneys activates angiotensin, increasing blood pressure through sodium and water retention and vasoconstriction. Vitamin D seems to have an inhibitory effect on this pathway. Research indicates that vitamin D helps regulate the RAAS, as lower vitamin D levels have been associated with higher angiotensin II and renin activity. Individuals with vitamin D deficiency can experience increased RAAS activity, potentially raising blood pressure, which supports a link between vitamin D and blood pressure control.
Hypertension is a widely recognized risk factor and comorbidity of Afib. Therefore the RAAS regulatory effects of vitamin D could be very beneficial for patients with atrial fibrillation.

Anti-inflammatory effects of Vitamin D
Vitamin D helps regulate the immune system by enabling immune cells to manage local levels of calcitriol. Calcitriol is the active form of Vitamin D which can alter the behavior of immune cells and cause anti-inflammatory effects. Adequate vitamin D is linked to higher levels of anti-inflammatory cytokines (IL-4 and IL-10) and lower levels of pro-inflammatory cytokines (IL-1 and IL-6). In contrast, vitamin D deficiency is associated with chronic inflammation, oxidative stress, and fibrosis all of which can result in cardiovascular issues including heart failure.
Although no causal relationships have been established between inflammation and Afib a strong association between these two has been seen. Inflammation is also considered a risk factor for Afib.
How Vitamin D deficiency may influence Afib risk
A meta-analysis including 13 studies with a total of 6519 cases of Afib among 74,885 participants, found that a vitamin D deficiency was associated with an increased risk of atrial fibrillation and postoperative atrial fibrillation.
Additionally, a study from Finland showed that for Afib patients with already normal to high baseline vitamin D levels, supplementation could still decrease the incidence of atrial fibrillation. A 27% decrease in incidence was seen compared to the control group. So even in patients with no deficiency, supplementation could be greatly beneficial.
There is no set dosage of vitamin D supplements that have been recommended for Afib patients specifically but the daily advised dosage for adults is between 15-20mcg.
Based on the mechanistic effects of vitamin D and also its tested positive effects on Afib patients, this supplement has great therapeutic potential. Thus supplementation could be an easy and beneficial tool for lowering the risk and incidence of atrial fibrillation.
References
Nso, N., Bookani, K. R., Metzl, M., & Radparvar, F. (2020). Role of inflammation in atrial fibrillation: A comprehensive review of current knowledge. Journal of arrhythmia, 37(1), 1–10. https://doi.org/10.1002/joa3.12473
Peruzzu, D., Dupuis, M. L., Pierdominici, M., Fecchi, K., Gagliardi, M. C., Ortona, E., & Pagano, M. T. (2022). Anti-Inflammatory Effects of 1,25(OH)2D/Calcitriol in T Cell Immunity: Does Sex Make a Difference?. International journal of molecular sciences, 23(16), 9164. https://doi.org/10.3390/ijms23169164
Aronow W. S. (2017). Hypertension associated with atrial fibrillation. Annals of translational medicine, 5(23), 457. https://doi.org/10.21037/atm.2017.10.33
Ajabshir, S., Asif, A., & Nayer, A. (2014). The effects of vitamin D on the renin-angiotensin system. Journal of nephropathology, 3(2), 41–43. https://doi.org/10.12860/jnp.2014.09
Zarzour, F., Didi, A., Almohaya, M., & Kendler, D. (2023). Cardiovascular Impact of Calcium and Vitamin D Supplements: A Narrative Review. Endocrinology and metabolism (Seoul, Korea), 38(1), 56–68. https://doi.org/10.3803/EnM.2022.1644
Reid, I. R., Mason, B., Horne, A., Ames, R., Clearwater, J., Bava, U., Orr-Walker, B., Wu, F., Evans, M. C., & Gamble, G. D. (2002). Effects of calcium supplementation on serum lipid concentrations in normal older women: a randomized controlled trial. The American journal of medicine, 112(5), 343–347. https://doi.org/10.1016/s0002-9343(01)01138-x
Chin, K., Appel, L. J., & Michos, E. D. (2017). Vitamin D, Calcium, and Cardiovascular Disease: A”D”vantageous or “D”etrimental? An Era of Uncertainty. Current atherosclerosis reports, 19(1), 5. https://doi.org/10.1007/s11883-017-0637-2
Laird, E., Ward, M., McSorley, E., Strain, J. J., & Wallace, J. (2010). Vitamin D and bone health: potential mechanisms. Nutrients, 2(7), 693–724. https://doi.org/10.3390/nu2070693
National Institute of Health, Office of Dietary supplements. Vitamin D, Fact Sheet for Health Professionals. (n.d) https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Okin, P. M., Hille, D. A., Wachtell, K., Kjeldsen, S. E., Julius, S., & Devereux, R. B. (2020). On-treatment HDL cholesterol predicts incident atrial fibrillation in hypertensive patients with left ventricular hypertrophy. Blood Pressure, 29(5), 319–326. https://doi.org/10.1080/08037051.2020.1782171
Roffe-Vazquez, D. N., Delgado, A. S. H., Castillo, E. C., Villarreal-Calderón, J. R., Gonzalez‐Gil, A. M., Enriquez, C., … & Elizondo‐Montemayor, L. (2019). Correlation of vitamin d with inflammatory cytokines, atherosclerotic parameters, and lifestyle factors in the setting of heart failure: a 12-month follow-up study. International Journal of Molecular Sciences, 20(22), 5811. https://doi.org/10.3390/ijms20225811
Liu, X., Wang, W., Tan, Z. et al. The relationship between vitamin D and risk of atrial fibrillation: a dose-response analysis of observational studies. Nutr J 18, 73 (2019). https://doi.org/10.1186/s12937-019-0485-8
Virtanen, J. K., Hantunen, S., Lamberg‐Allardt, C., Manson, J. E., Nurmi, T., Uusitupa, M., … & Tuomainen, T. (2023). The effect of vitamin d3 supplementation on atrial fibrillation in generally healthy men and women: the finnish vitamin d trial. American Heart Journal, 264, 177-182. https://doi.org/10.1016/j.ahj.2023.05.024
Do you know someone who might be interested in this?